CASE STUDY
Planning a Total Knee Replacement and Tibial Osteotomy to Replace and Realign the Knee Joint
Orthopaedic Surgeon Dr. Neville Strick used Materialise OrthoView orthopaedic planning software to better understand the anatomy of a patient with a history of rickets and plan a procedure to replace and realign the knee joint to relieve pain and restore mobility.
The challenge
Determine a treatment plan for a patient with a history of rickets
The patient (male, age 53) has a history of hypophosphatemic rickets. The associated bone abnormalities and leg malalignment were addressed by bilateral closing wedge tibial osteotomies when the patient was approximately 40 years of age. The patient was later experiencing pain in both knees and was having difficulty walking.
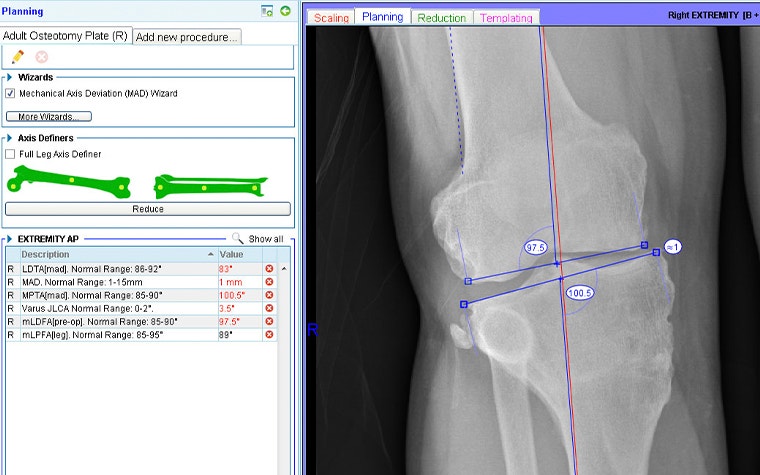
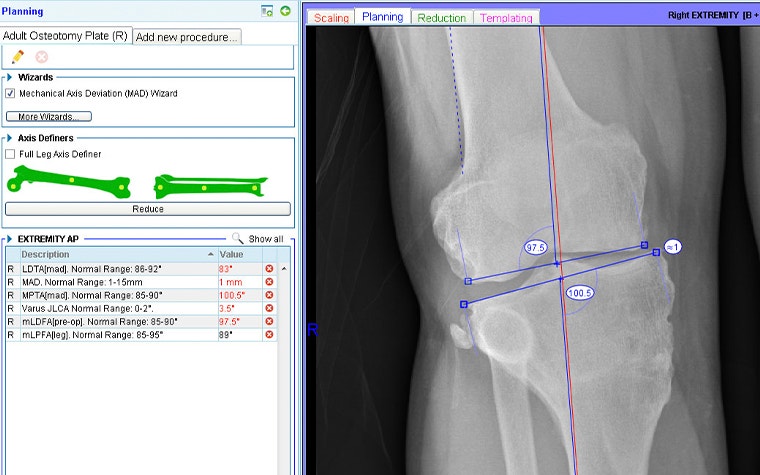
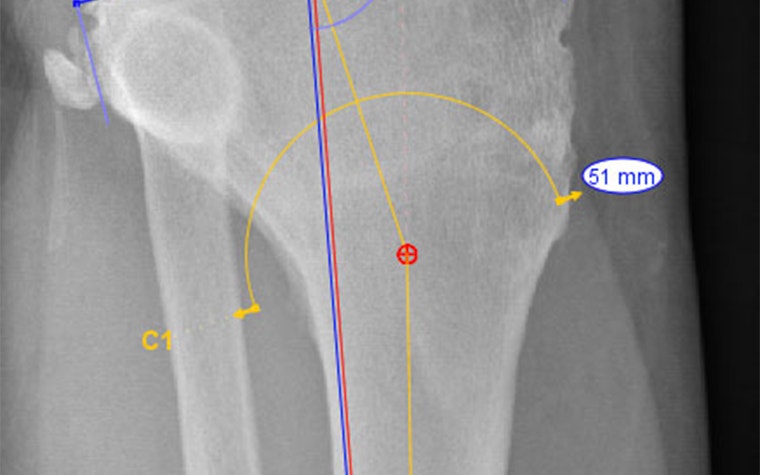
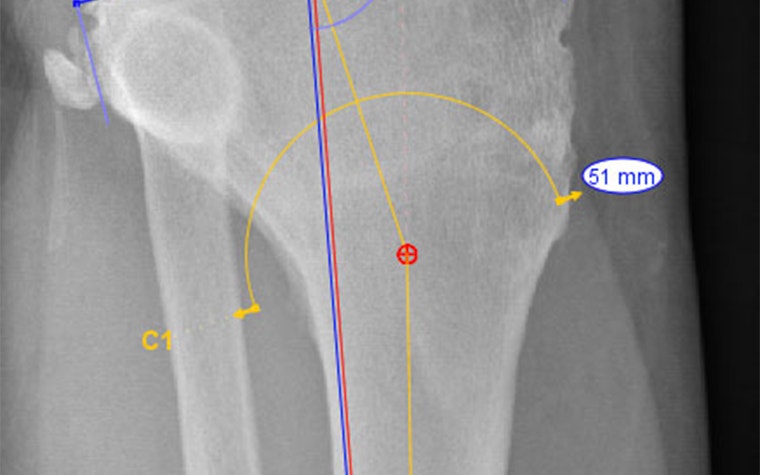
Considering the right leg first, examination of the long-leg weight-bearing AP X-ray shows good mechanical axis alignment but a significantly oblique knee joint line (figure 1). It was apparent that mild osteoarthritis had become worse over time, presumably as a result of the joint obliquity.


With the AP long-leg X-ray loaded into the OrthoView application, the surgeon used the Mechanical Axis Deviation (MAD) Wizard from the Limb Deformity Correction (LDC) Module.
This confirmed that the knee joint line convergence angle was outside of normal range. Specifically, using the nomenclature developed by Paley et al., the mLDFA (mechanical Lateral Distal Femoral Angle) and MPTA (Medial Proximal Tibial Angle) were 7.5 degrees and 10 degrees outside of normal range, respectively.
All values out of range are highlighted in red in figure 2.
Surgical strategies were then considered. While combined femoral and tibial osteotomies could have corrected the joint obliquity, the joint surfaces were judged to be too badly damaged.
A total knee replacement (TKR) would replace the worn joint surfaces; however, correct alignment would not be possible with a TKR alone since this would involve cutting ligaments. Therefore, a combined proximal tibial osteotomy and TKR were proposed and the subject of a detailed preoperative plan.
The solution
Planning and templating using OrthoView X-ray planning software
The first goal of the planning phase was to demonstrate the feasibility of the proposed, and relatively complex, surgery. Important questions included:
- What would be the effect of the tibial osteotomy on overall leg alignment and length?
- What would be the impact of the proposed TKR cuts and tibial osteotomy on the soft tissues?
- Would the surgery result in good stability and be likely to heal well?
Using the axis definers in OrthoView’s LDC Module, a CORA was established which identified the magnitude of the angulation correction required as 18 degrees. A cut was added, a dome cut being preferred to an opening wedge as the latter would be too large and unstable in this case. An inverted dome cut was preferred over the standard orientation (as shown) to make it easier to avoid the patellar tendon.
On-screen ‘reduction’ identifies the following:
- No postoperative change in leg length
- An indication of the saw blade radius
- Location of where the mechanical axis passes through the knee joint. Note: Although medialized, this was judged to be acceptable.


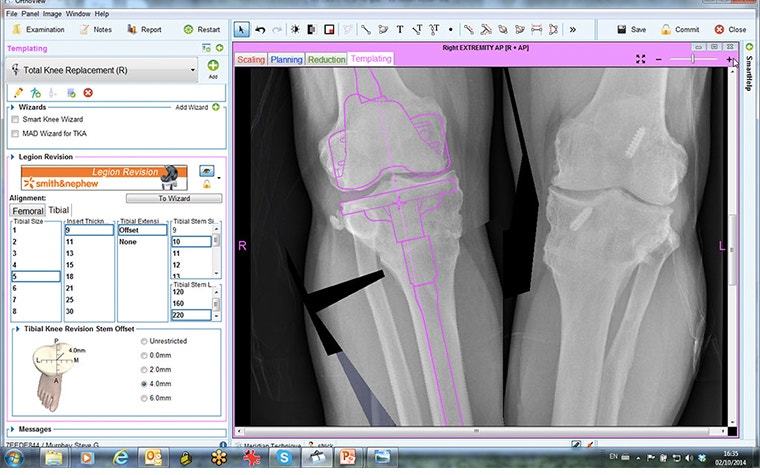
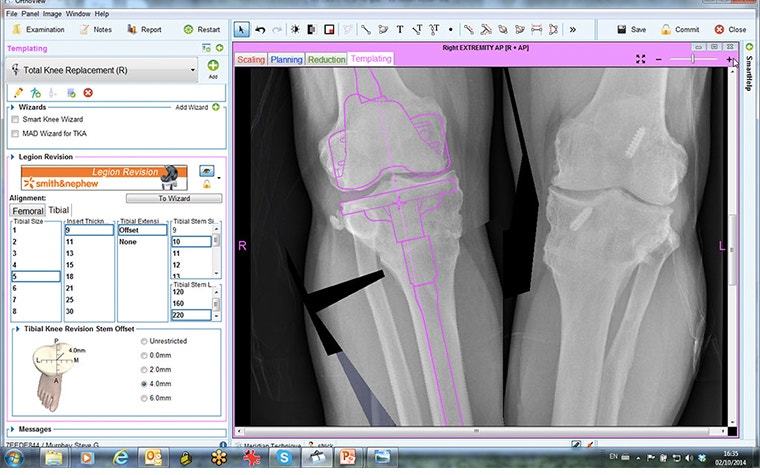
Having completed planning for the tibial osteotomy, the next phase of the plan was to use OrthoView’s ‘Add New Procedure’ feature to plan for the TKR.
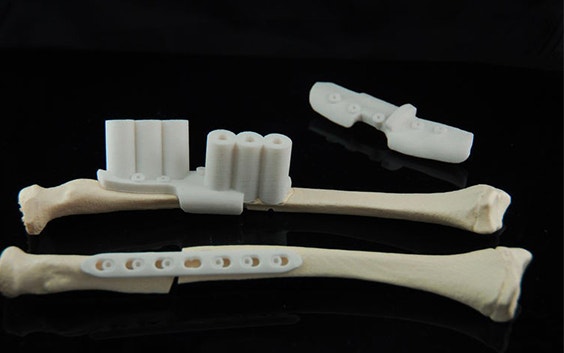
A revision system, the Smith & Nephew Legion, was chosen since the optional offset stem would be used to help with fixation of the tibial osteotomy. Since the OrthoView digital orthopaedic template for the Smith & Nephew Legion behaves as a complete interconnected system, mimicking the behavior of the actual implant, templating for the necessary stem offset is possible.
The resulting preoperative plan provided not only the sizing of the components but also the positioning of the intra-articular cuts and insights into how these would subsequently affect ligament balancing.
The result
Effective treatment plan with a positive patient outcome
- Surgery: The trials for the knee replacement were fitted first, and the knee joint was determined to be a good functional fit — ligament balance with the cuts required being a major consideration.
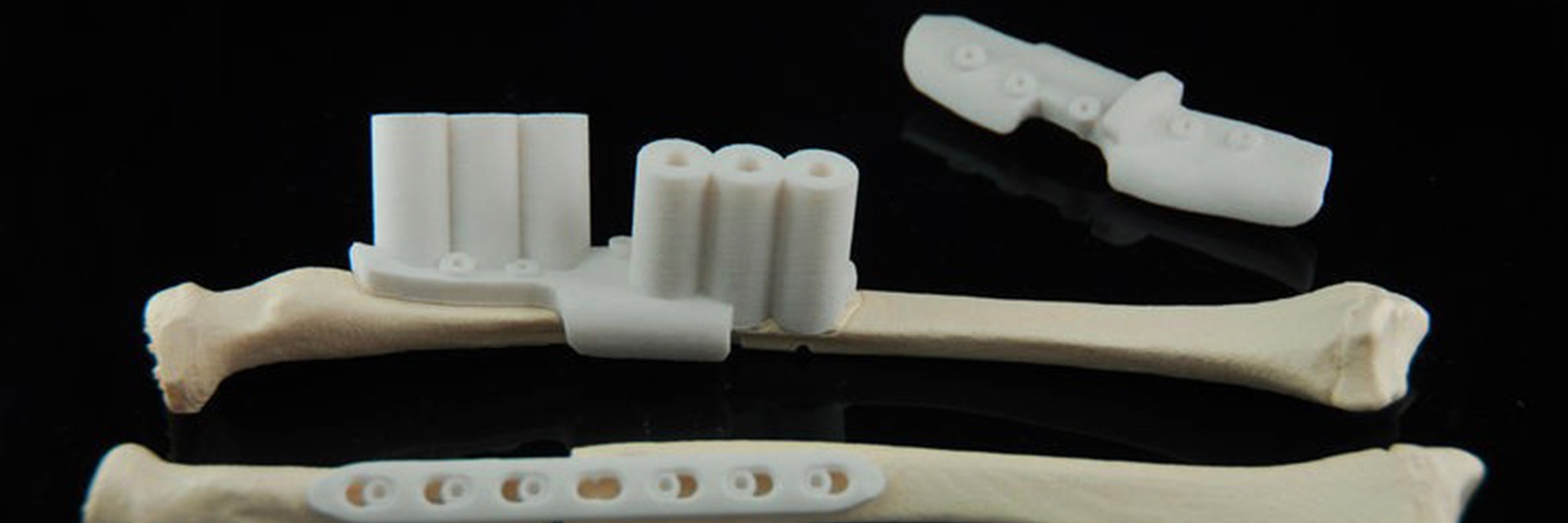
The osteotomy was followed by disruption of the fibula to perform the inverted dome osteotomy and the use of the revision stem to anchor the bone, along with a small plate for added support. Bony union was anticipated to be adequate due to the nature of the dome osteotomy.
- Outcomes: At his six-week return assessment, the patient was pleased with the progress and results, and he was preparing for the left lower limb to also be repaired to improve function via a similar method.
The union is progressing well with subsequent follow-up, and the patient remains very happy with the outcome.


Clearly, preoperative planning is essential in a case like this. In times gone by, planning this surgery would have required the surgeon to trace the X-ray images and apply multiple bits of paper to go through the above steps.
This study describes a ‘final draft’ of the plan but the software allows many ‘what if’ scenarios, with the ability to very easily return to the beginning of a step. In a case like this, it is gratifying when the templating steps match the intra-operative steps very closely, and having used OrthoView software for multiple complex cases, it's safe to say this is a consistent outcome for the surgeon: "The more complex the case, the more useful the planning software is."
Materialise OrthoView is a digital templating solution used by orthopaedic surgeons to create detailed preoperative plans quickly and easily from digital X-ray images. Materialise OrthoView facilitates digital planning and templating for joint arthroplasty and revisions, trauma, limb deformity correction, osteotomy and spinal assessment and is chosen by hospitals worldwide to complete their target of film-free radiology.
Share on:
This case study in a few words
Healthcase
OrthoView
Effective preoperative planning
Higher accuracy and predictable patient outcomes