INTERVIEW
How a Quality Management System Is Helping a 20+ Year Old 3D Lab Scale Up While Retaining Excellence
Queen Elizabeth Hospital Birmingham, a pioneer of 3D labs at the point-of-care, was the first to have a PolyJet printer in UK hospitals. They are also the largest maxillofacial prosthetics center in the UK. We talked with Stefan Edmondson, a Maxillofacial Prosthetist and Consultant Clinical Scientist at the 3D virtual surgical planning department, about how the 3D lab has evolved with innovative technology and techniques over the 22 years he has worked there. And now, how the quality management system has changed everything since it was implemented.
How has 3D planning and 3D printing been integrated into your work?
It has helped the workflow with how we diversified as a profession. Many of the analogue techniques that we were always doing have allowed us to evolve with the digital side of things. And it's a plus that it's saved money and time. While it has been an evolutionary process, we've been one of the departments that have learned from our mistakes. We now support other departments starting up to come see the systems we have in place. We've had to evolve to be as streamlined and financially viable as possible in a patient-specific hospital and point-of-care settings.
For what applications do you use 3D?
We use Materialise 3-matic medical software for orthognathic, burn patients, and freeform as well for the design aspect*. Materialise Mimics software is ideal for segmenting all the DICOM data for orthopaedics, burns, plastics, maxillofacial, etc. Whatever the format is, in DICOM, if it's cardiovascular or orthopaedic, if that data can be segmented and used for a personalized item, then that's the whole spectrum. And everybody can have a 3D CT scan and DICOM. It's an open Pandora's Box, and the possibilities are enormous.
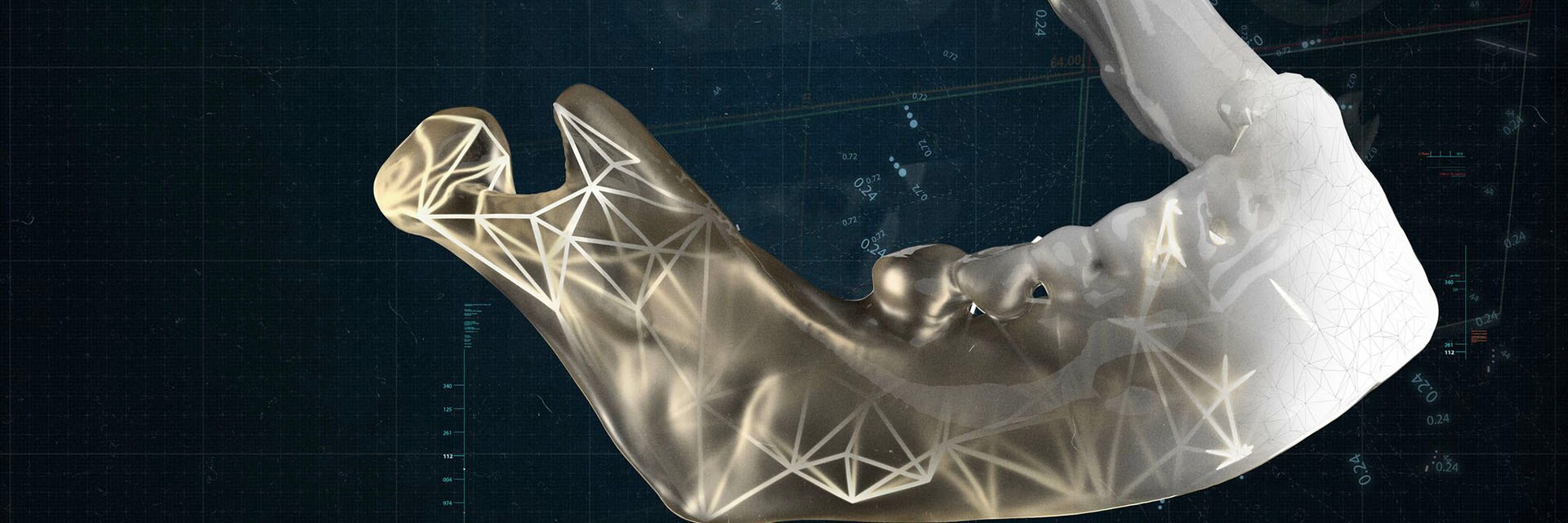
A tour of the 3D lab at Queen Elizabeth hospital and the different possibilities for usage.
How many people are working there and in what ways?
When we're up to full capacity, we have 13 people. We run in a different format from other hospitals because we specialize in facial prosthetics. Somebody has to work at it five days a week. This is why we are one of the first in the UK to appoint a biomedical and application engineer as a full-time position. We look after four hospitals that have thousands of employees. We have a staff structure with lead specialists in a certain area, whether it be orbits for the eyes, burns, head and neck cancer, or orthognathic neurosurgical for cranioplasty.
What benefits have you experienced from having this 3D lab at the point of care?
We can send orders out to an external company to be 3D-printed or have a virtual surgical plan, but that all takes a lot of time. However, it only takes 24-48 hours if we can do it ourselves. It just makes sense to have everything on-site and within easy access.
For example, we are one of the largest head and neck cancer units in Europe and have a long list of patients that only got longer after the pandemic pushed back appointments. However, when we have a cancellation, we can plug that hole in the schedule with someone else if we can get a plan done quickly. This would be nearly impossible if we had to account for the time it would take to send out to an external company.
Can you share some differences from your workflow before you had a 3D lab at the point of care?
The integration between the application engineers and the surgeon is the big difference. Everything is personal — if you can sit in a room with somebody, it makes it more accessible.
Over the years, you have surgeons who would request a model because they can. And many of those 800-euro models end up as paperweights or in the boot of their cars. Some surgeons don't realize that they can stop by and see it in PROPLAN — that they can spin it around and see segments on the screen or that we can even send them a screenshot. So, part of the job is educating them about the possibilities of the work we can do in the lab.
How do you ensure the integrity of your work — is there a quality management system (QMS), and if so, what is the typical workflow?
We have had a QMS and tracking and traceability within our department for about two years. We're currently going through our BSI ISO 13485 for implantable devices. Andrea, the office manager, logs everything from the primary patient referral; everyone has a storybook. For example, if it's a burn patient, everything we do with the scanning, what we print the facial splint with, lot numbers to product numbers, 3D resins, everything is recorded and uploaded. Every single meeting with surgeons is documented so that when they are in the theater, they can see those control drawings within that patient's storybook.
The QMS has massively changed how we work, and it is now a regulatory part of what we do. We are now required to be registered as a maxillofacial prosthetic department through the MHRA. Before QMS, things could have been overlooked and might not have been documented properly.
How is having a biomedical engineer in-house beneficial to the 3D lab?
It's hugely beneficial because before we had a biomedical/application engineer, it was somebody who was being pulled between two areas, whereas Millie, our new biomedical engineer, can just sit down and design. She communicates with the surgeons, logs into MDT (multidisciplinary team) meetings, and does virtual platforms. So that just gives us that extra resource to know that everything's being done how it should be, and within the QMS.
How has 3D printing and 3D planning affected patient care?
It has transformed patient care through accuracy, speed, cost, and quality. It's turned the medical field upside down, especially with the medical application of engineering and the personalized, implantable devices, and the accuracy of the finished product. In one sentence, the predictability is predictable. Whereas before, it really wasn't. I personally have seen it along the way.
What advice would you give to other hospitals that are interested in starting their own 3D labs?
Don't make the mistakes we've made. Come and see us, go and look at other units. If you're just printing 3D models, fine. But if you're doing a personalized device associated with that, investigate it financially and cost-effectively. Some printers are heavily expensive to maintain, and there's no point in spending a lot of money if it's cheaper to have it all sent out at the end of the day. The fact is that there's a patient at the end of it, and we're not hiding any trade secrets of what we're doing at all.
What are your next challenges in terms of 3D?
I'd certainly like to branch out in different aspects within 3D printing, such as metal printing. Some of the surgeons would like to develop new techniques. And that's what we are here for — if you want to try something new, that's where you have to lean into us. We can adapt.
After 20 years of rapid growth and expansion, the Queen Elizabeth 3D lab is continuing to improve its processes. There have been numerous benefits, such as being able to fill last-minute schedule cancellations with a new patient and being able to work with surgeons to create innovative plans. With the QMS in place for the last few years, and the structure of people they have in place, they are ready to scale up while retaining the quality and attention needed.
*The safety and effectiveness of designed medical devices should be guaranteed by the designer.
L-102622
Share on:
You might also like
Never miss a story like this. Get curated content delivered straight to your inbox.