EXPERT INSIGHT
Why Enabling Technology Is Critical for Personalized Knee Alignment

Total knee arthroplasty (TKA) has revolutionized patient care for degenerative knee joint disease. While the surgery is successful in most cases, around 20% of patients report dissatisfaction with their knee after surgery. Personalized alignment for TKA has grown in popularity in recent years, with the aim of improving outcomes for patients. In this article, we discuss how enabling technologies, such as 3D preoperative planning and surgical guides, may help achieve optimal results when choosing an alignment philosophy that stays closer to the natural anatomy of a patient's knee.


The growing trend towards personalized alignment for total knee arthroplasty
Total knee arthroplasty (TKA) is one of the most common joint replacement surgeries, with around 2.6 million procedures performed annually worldwide. The number of primary TKA procedures is projected to grow by 85% by 2030 to 1.26 million procedures per year in the US alone[1] .
Most patients undergoing TKA surgery report satisfactory results. However, a significant proportion — around 20% — remain unsatisfied with their outcomes following surgery. Comparisons with total hip replacement show that the Forgotten Joint Score for TKA is significantly lower and that fewer patients feel their knee feels “natural” after surgery (56% vs 22%)[2],[3] .
Improving functional outcomes, decreasing pain, and enhancing patient satisfaction following TKA has become a key focus of ongoing research and technological advancements. Substantial improvements over the past two decades in implant designs, surgical techniques, and postoperative rehabilitation programs have improved implant survival rates. However, they have not decreased dissatisfaction among patients[4],[5],[6],[7].
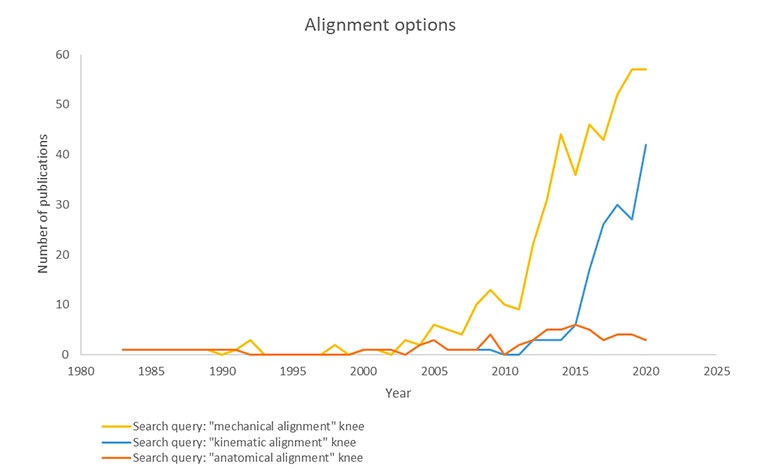
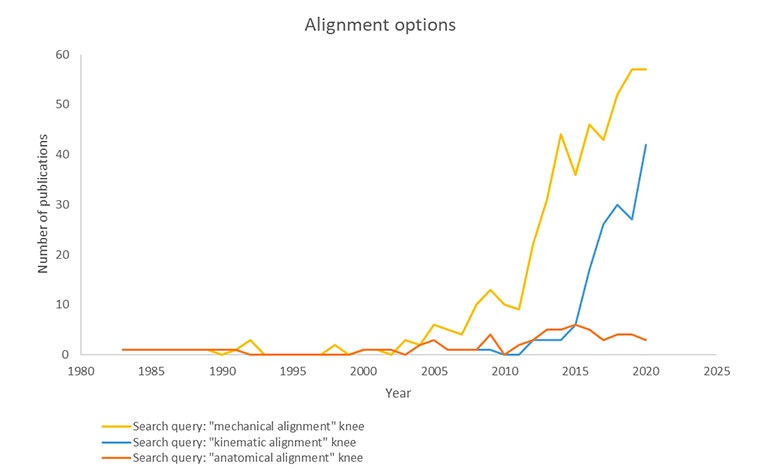
Several clinical studies have shown that malalignment has a significant impact on implant failure rates, and it is one of the main causes of pain and instability[8],[9],[10]. Until now, the optimal alignment for TKA has remained an unanswered question in the orthopaedic community. Mechanical alignment (MA) remains the most commonly used technique but has become seen as one of the potential causes of patient dissatisfaction rates and residual symptoms[11]. Personalized alignment has emerged as a growing trend. There is a consensus on the necessity to use enabling technologies when opting for this approach.
Personalized alignment may improve outcomes for patients
Mechanical alignment with a neutral hip-knee-ankle (HKA) angle of 180° has long been the gold standard in TKA. Uncomplicated MA in TKA has demonstrated long-term implant survival, but functional outcomes are variable[12].
In 2011, Bellemans et al. demonstrated that every patient's anatomy is unique, with a wide range of hip-knee-angle variations across the population. Restoring neutral alignment may not be the best option for patients who have always had a natural varus[13]. For this reason, the concept of MA and its 'one size fits all' approach has become the subject of debate in the orthopaedic community. MA is limited in its ability to replicate the anatomy and kinematics of a patient's natural knee[14].
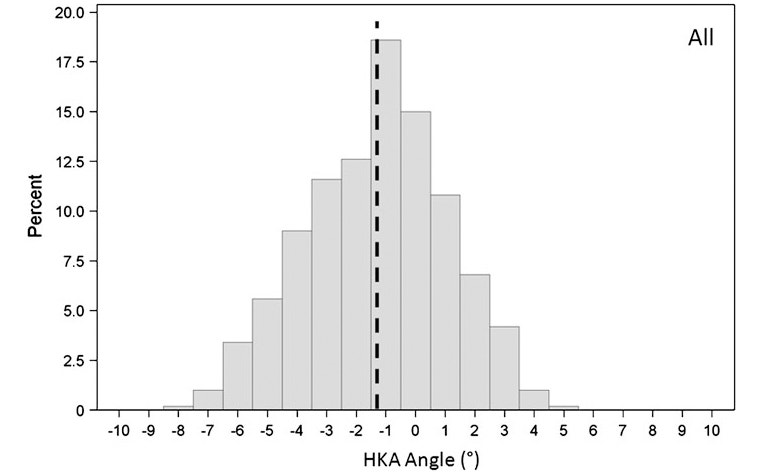
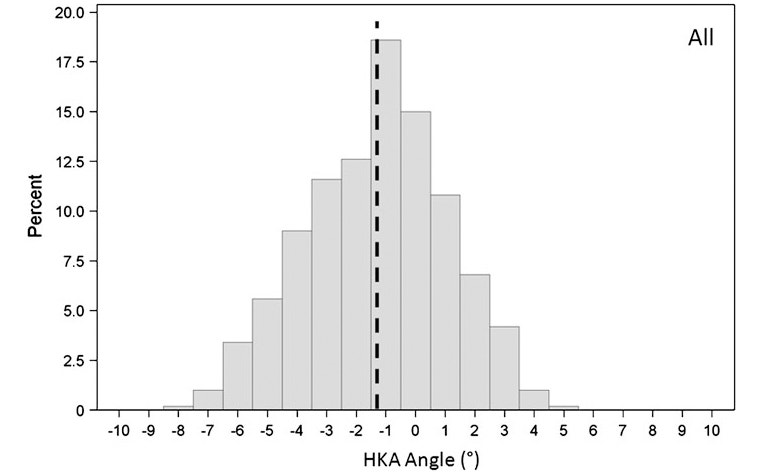
Therefore, new personalized alignment methodologies have been introduced with the aim of improving functionality for patients via closer reproduction of their native knee alignment. Methodologies such as adjusted mechanical, kinematic, and restricted kinematic alignment are gaining broader acceptance.
Each of the three alignment philosophies requires a different technique, as summarized below. (Sources: Lustig et al., Winnock et al. )
Adjusted mechanical alignment:
- Adapts the conventional MA technique to under-correct the constitutional frontal deformity (varus or valgus) to a maximum of 3°
- Implant positioning adjustment is made on the femoral side; tibial implant stays mechanically aligned
Kinematic alignment:
- The aim is knee resurfacing with the restoration of the pre-arthritic anatomy and preservation of the soft-tissue envelope
- Full anatomic positioning of the TKA implants along three kinematic axes and joint lines of the native joint
Restricted kinematic:
- Considered a hybrid option between MA and kinematic alignment for patients with substantial deformities
- The algorithm involves modifying bone cuts to a 'safe range'
While no conclusive clinical studies have demonstrated the superiority of one planning philosophy over another, a common consensus is that consistently reproducing a personalized alignment is difficult. The use of enabling technologies, such as advanced imaging and 3D planning software, personalized guides, navigation, or robotics is considered critical to success[15],[16],[17].
Enabling technology provides the required precision for personalized alignment
Conventional instruments were originally designed and developed to execute mechanical alignment. A lack of proper assessment tools to find the most suitable alignment for each patient makes following a personalized alignment philosophy challenging. Limited insights into the 3D anatomy of the knee during surgery will further increase the amount of variability or outliers15,16,17.
In addition, this may result in dangerous outcomes when a desired personalized alignment is situated at the boundaries of the safe zone. For instance, a +/- 5 degree variability on a patient with a 3-degree varus, which is corrected to a 3-degree varus, may result in an 8-degree varus.
Therefore, it is even more important to reproduce the alignment precisely when opting for a personalized alignment approach.
Both precision and accuracy are needed to execute the ideal alignment philosophy
Precision is the ability to achieve consistent results without outliers. Accuracy is the capacity to achieve a predefined target. In this context, the target is perfect alignment for each patient. As such, both accuracy and precision are necessary to achieve the optimal alignment for each patient consistently.
To determine the right target, i.e., the right alignment for each patient, outliers need to be reduced as they can cause indecisiveness when the results overlap. To address this, studies must be performed to compare the outcomes for different alignment philosophies using precise enabling technology.
Personalized guides are a proven precision enabler
3D planning provides an in-depth, three-dimensional assessment of the patient's anatomy. This includes the patient's wear patterns and alignment angles. According to clinical judgment, this information can then be used to optimize the position of the tibial and femoral components in the coronal and sagittal planes. The use of enabling technologies, such as personalized guides, allows surgeons to transfer these planned alignment angles into the operating theater with precision.
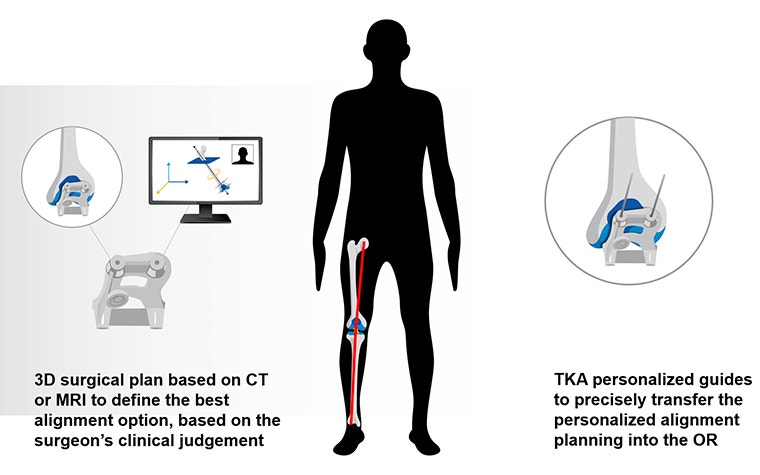
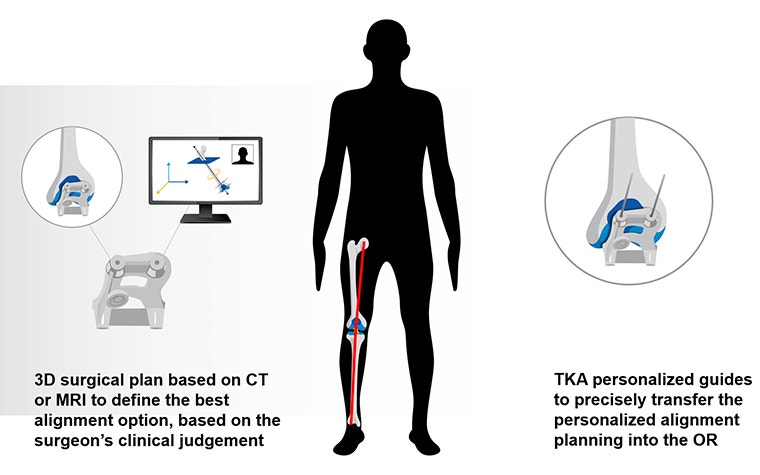
Over the past 12 years, studies have demonstrated that a surgical plan is more reproducible, i.e., with fewer outliers in different planes, using 3D planning and personalized guides in comparison to standard instruments[18],[19]. In addition, personalized guides are a cost-efficient solution and easily accessible to any surgeon wanting to enhance accuracy and precision, regardless of their preferred alignment philosophy.
[1] Sloan M, Premkumar A, Sheth NP. Projected Volume of Primary Total Joint Arthroplasty in the U.S., 2014 to 2030. J Bone Joint Surg Am. 2018;100(17):1455-60.
[2] Nam D, Nunley RM, Barrack RL. Patient dissatisfaction following total knee replacement: a growing concern? Bone Joint J. 2014;96-b(11 Supple A):96-100.
[3] Thienpont E, Vanden Berghe A, Schwab PE, Forthomme JP, Cornu O. Joint awareness in osteoarthritis of the hip and knee evaluated with the 'Forgotten Joint' Score before and after joint replacement. Knee Surg Sports Traumatol Arthrosc. 2016;24(10):3346-51.
[4] . Siddiqi A, Horan T, Molloy RM, Bloomfield MR, Patel PD, Piuzzi NS. A clinical review of robotic navigation in total knee arthroplasty: historical systems to modern design. EFORT Open Rev. 2021;6(4):252-69.
[5] Riviere C, Iranpour F, Auvinet E, Howell S, Vendittoli PA, Cobb J, et al. Alignment options for total knee arthroplasty: A systematic review. Orthop Traumatol Surg Res. 2017;103(7):1047-56.
[6] Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KD. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res. 2010;468(1):57-63.
[7] Baker PN, van der Meulen JH, Lewsey J, Gregg PJ, National Joint Registry for E, Wales. The role of pain and function in determining patient satisfaction after total knee replacement. Data from the National Joint Registry for England and Wales. J Bone Joint Surg Br. 2007;89(7):893-900.
[8]Gromov K, Korchi M, Thomsen MG, Husted H, Troelsen A. What is the optimal alignment of the tibial and femoral components in knee arthroplasty? Acta Orthop. 2014;85(5):480-7.
[9] Ritter MA, Davis KE, Meding JB, Pierson JL, Berend ME, Malinzak RA. The effect of alignment and BMI on failure of total knee replacement. J Bone Joint Surg Am. 2011;93(17):1588-96.
[10] Schroer WC, Berend KR, Lombardi AV, Barnes CL, Bolognesi MP, Berend ME, et al. Why are total knees failing today? Etiology of total knee revision in 2010 and 2011. J Arthroplasty. 2013;28(8 Suppl):116-9.
[11] Lustig S, Sappey-Marinier E, Fary C, Servien E, Parratte S, Batailler C. Personalized alignment in total knee arthroplasty: current concepts. SICOT J. 2021;7:19.
[12] Lustig S, Sappey-Marinier E, Fary C, Servien E, Parratte S, Batailler C. Personalized alignment in total knee arthroplasty: current concepts. SICOT J. 2021;7:19.
[13] Bellemans J. Neutral mechanical alignment: a requirement for successful TKA: opposes. Orthopedics. 2011;34(9):e507-9.
[14] Hirschmann MT, Becker R, Tandogan R, Vendittoli P-A, Howell S. Alignment in TKA: what has been clear is not anymore! Knee Surgery, Sports Traumatology, Arthroscopy. 2019;27(7):2037-9.
[15] Goyal N, Patel AR, Yaffe MA, Luo MY, Stulberg SD. Does Implant Design Influence the Accuracy of Patient Specific Instrumentation in Total Knee Arthroplasty? J Arthroplasty. 2015;30(9):1526-30.
[16] Stronach BM, Pelt CE, Erickson J, Peters CL. Patient-specific total knee arthroplasty required frequent surgeon-directed changes. Clin Orthop Relat Res. 2013;471(1):169-74.
[17]Pietsch M, Djahani O, Hochegger M, Plattner F, Hofmann S. Patient-specific total knee arthroplasty: the importance of planning by the surgeon. Knee Surg Sports Traumatol Arthrosc. 2013;21(10):2220-6.
[18] Noble JW, Jr., Moore CA, Liu N. The value of patient-matched instrumentation in total knee arthroplasty. J Arthroplasty. 2012;27(1):153-5.
[19] Pietsch M, Djahani O, Zweiger C, Plattner F, Radl R, Tschauner C, et al. Custom-fit minimally invasive total knee arthroplasty: effect on blood loss and early clinical outcomes. Knee Surg Sports Traumatol Arthrosc. 2013;21(10):2234-40.
L-102220-01
Share on:
You might also like
Never miss a story like this. Get curated content delivered straight to your inbox.
