EXPERT INSIGHT
Catheter Training for Pediatric Cardiology Using Pulsating 3D-Printed Hearts

Effective medical training relies on the ability to perform practice treatments repeatedly. To enable particularly realistic catheter training for the interventional treatment of congenital heart defects the Department of Pediatric Cardiology at the Ludwig Maximilian University (LMU) Hospital in Munich came up with a novel solution. They developed 3D-printed models of children's hearts afflicted with heart defects. The latest generation of 3D-printed models can even beat like a real heart. The clinical team used Materialise's Mimics Innovation Suite software package to develop and modify the heart models.
The diagnosis and interventional treatment of congenital heart defects in children using catheter technology requires not only a detailed knowledge of the anatomy. It also requires analyzing potential problems, the necessary steps to correct them, and in particular, an enormous amount of dexterity when handling the catheter. The instrument must be guided extremely sensitively through the smallest spaces, and every intervention must be securely seated. However, there is no realistic training simulation set-up at this moment - neither for children's hearts nor for congenital heart defects. Unlike adult hearts, where there are at least virtual reality simulation systems for addressing typical adult diseases, education and training or the operation of children’s hearts still take place almost exclusively on humans.
For Prof. Nikolaus Haas, MD, this is a situation that needs to be improved. The Director of the Department of Pediatric Cardiology and Pediatric Intensive Care Medicine at LMU Hospital and President of the German Society for Pediatric Cardiology and Congenital Heart Defects (Deutsche Gesellschaft für Pädiatrische Kardiologie und angeborene Herzfehler e.V.), says "The current approach to the apprenticeship model is not only time-consuming and dependent on the motivation of the trainer, but also on the disease patterns, procedures, and technology that are presented to trainees during their training period.
“Methods and instruments are constantly evolving. Practicing physicians repeatedly find themselves in the embarrassing situation of not being able to master certain procedures and new instruments as confidently as would be desirable to ensure the maximum level of patient safety.
"In addition, we occasionally fail to fulfill our lifelong educational function, as young, dedicated colleagues do not have sufficient opportunities to perform catheter treatments independently, even though our long-term educational guidelines actually prescribe this."
Makeshift objects such as animal hearts or self-constructed scenarios from laboratory materials, such as tubes and balloons (which have been used sporadically up to now), are problematic and not very satisfactory. The ethics committee must approve their use in animal experiments. In addition, the organs are usually healthy, and therefore, do not provide the opportunity to practice interventions for congenital heart defects. The self-built scenarios, on the other hand, are far too unrealistic for in-depth training scenarios and can only serve as a basis for the initial, basic exercises.
Against this background, the idea of developing 3D-printed children's hearts specifically for training purposes was born at LMU Klinikum. Digital adaptations can be used to create a variety of models with different heart defects. Such replicas, adapted to the training objectives, offer physicians the opportunity to practice the treatment of typical clinical pictures as well as new instruments and procedures. Being able to do so repeatedly without risk, results in an enormous boost in confidence. Since the training models can be used multiple times and a new patient scan is not necessary for every heart defect, they have a long-term cost advantage over patient-specific representations. At the same time, they save young patients from unnecessary exposure to radiation and sedation, as no patient scans are required to produce new models using the digital modeling method.
From rough model to beating artificial heart
The path to pulsatile pediatric heart models was achieved through several generations of models. For the very first 3D-printed training models, the hospital team first assembled silicone tubes and plates to create a three-dimensional simplified representation of the heart with its main structures. "We used computed tomography to generate a 2D image stack of this assembly and then reconstructed a 3D-printable model from it," said Carina Hopfner, the engineer in charge of 3D printing at LMU Klinikum. "To convert the image data into a 3D model, we used Materialise's Mimics Innovation Suite, which allowed us to virtually complete the replica. Among other things, we used it to scale, smooth, and close surface defects," Carina continued. Finally, the simplified heart model was additively manufactured in one piece from a flexible, silicone-based tissue-like material.
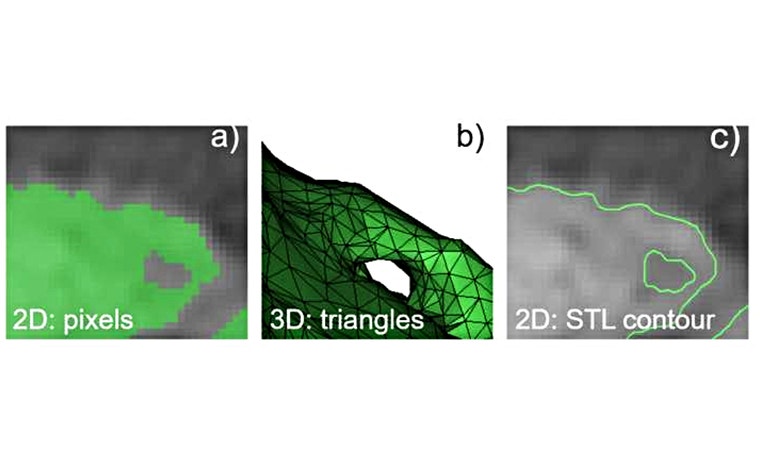
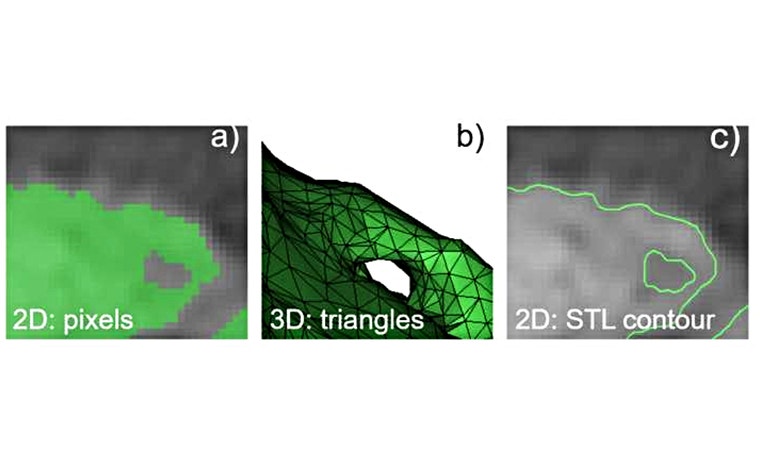
To create more realistic replicas of the human heart, the clinical team reconstructed next-generation pediatric heart models from anonymized CT or magnetic resonance imaging (MRI) scans of real patients. To do this, contrast-enhanced blood was tagged in the 2D images and then translated into a 3D volume describing the inner surface of the heart. Mimics Innovation Suite was used to create a realistic heart model by incorporating the uniform thickness around blood volume, the typical cavities, and the vascular structures found in the heart.
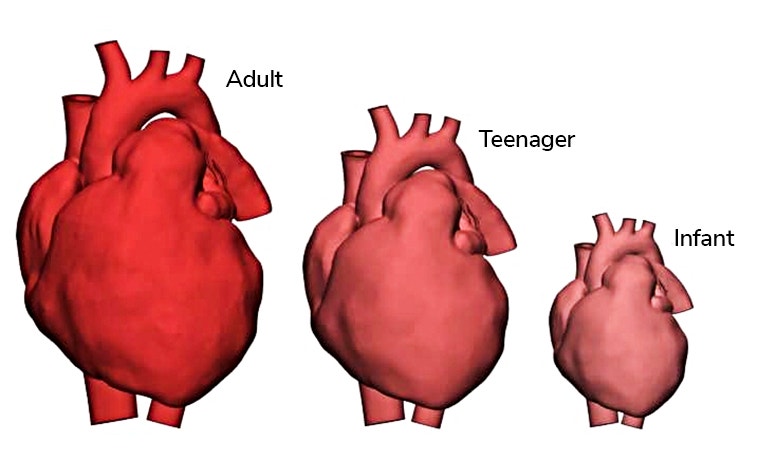
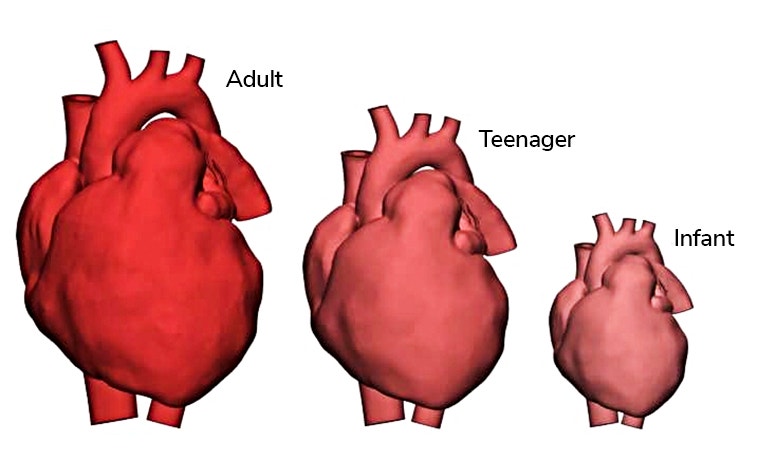
"We then scaled the virtual heart to different sizes of children's hearts and added various congenital defects — including holes in the cardiac septum, constrictions of vessels, or deformed structures. To do this, we primarily used tools from the design module in Materialise 3-matic. The 3D printing software, which is part of Mimics Innovation Suite, allows the entire unit as well as individual elements of the model to be scaled and surfaces, shapes, and wall thickness to be flexibly and precisely changed in the desired way," emphasized Carina. With collaboration between medical professionals and the engineer, the features of the models were gradually made more and more realistic. Finally, the models of the heart and the large vessels were 3D printed in the flexible material that was also used for the first-generation models.
The final step on the way to imitating a real human heart was to make the artificial heart pulsate realistically. To do this, the clinic team first integrated a heart valve into the existing static models using the design module in 3-matic. Since heart valves can only be captured inaccurately during CT scans, they were initially missing from the models. The 3D-printed heart representations, which were then optimized once again, were then connected by the staff involved to a closed, circular system of silicone tubes filled with water. A connectable pulsatile drive unit simulates the heartbeat in training situations.


"Materialise's Mimics Innovation Suite was of immense benefit in implementing the project. The software package is already the standard solution for converting medical image data into 3D-printable models, especially when creating personalized heart models. In particular, the 3-matic software included in it, with its numerous automated and semi-automated functions, helps to efficiently modify existing three-dimensional models, even at the mesh representation level. The possibilities are truly impressive. Without the Materialise solutions, the realization of the heart models would have been much more difficult," stated Carina.
Positive feedback after testing in real clinical environments
Both the static and pulsatile pediatric heart models, with the various virtual malformations built-in, were tested as part of a research project on educational practice in various real clinical environments in Germany and Austria. Among the clincs were the LMU Klinikum and the Pediatric Heart Center at the Medical University of Vienna. Outside Europe, extensive practical tests with static replicas took place at the Ayder Referral Hospital of the University of Mekelle in Ethiopia. With its technological challenges and staff that must cope with demanding training conditions, the facility is a good gauge to test the universal, ease of use of these 3D-printed heart models.
"Feedback from the workshops held so far for students, residents, and experienced pediatric cardiologists using the 3D-printed heart models has been overwhelmingly positive," said Prof. Dr. Haas. "Among other things, the experienced players emphasize the realistic character of the replicas, including the haptic and anatomical replication as well as the procedural simulation of the interventions. I can confirm this positive finding. Entire intervention teams can gain confidence in this catheter application under realistic conditions."
University Prof. Dr. Ina Michel-Behnke from the Pediatric Heart Center Vienna substantiates the benefits: "We trained our students and postgraduates who are not regularly involved in interventions on-site in the cath labs, using the 3D heart models, and could see a rapid improvement in handling skills, as well as a reduction in the duration of the procedure and radiation. The trainee pediatric cardiologists felt much more comfortable with their first patient cases after being introduced to them through this module of interventional training and were very relieved to be able to keep the radiation dose to their patients low."


Prof. Dr. Haas believes the new heart models are groundbreaking: "Because of the numerous benefits associated with such 3D-printed models, I believe that training on them should be an integral part of pediatric cardiology training. Training on them can be carried out regularly in any hospital equipped with a cardiac catheterization laboratory without a major financial and technological outlay. As a result, hand movements and processes are internalized faster and better."
L-102507-01
Share on:
You might also like
Never miss a story like this. Get curated content delivered straight to your inbox.
