CUSTOMER STORY
Clinicians Gain Confidence from an Innovative 3D-Printed Simulator for Complex Transcatheter Edge-to-Edge Repair
Mitral regurgitation (MR) is one of the most common forms of heart valve disease. It's a condition in which the mitral valve's leaflets do not close properly, causing a backward flow of blood from the left ventricle to the left atrium. Cue in TEER, also known as transcatheter edge-to-edge repair. It's a procedure that allows the safe and effective reduction of MR in high-risk patients by inserting a catheter through a blood vessel up to the heart. A clipping device is inserted through the catheter, and the valve leaflets are clipped together to improve closure and decrease leaking.
Compared to open heart surgery, it is minimally invasive and has a shorter patient recovery time. However, it is a complex procedure for clinicians. It requires precise catheter manipulation and positioning to ensure a successful placement of the mitral valve clip, and navigating the transseptal puncture for clip deployment is challenging.
Answering a clinical request with 3D technology
We spoke to Michele Bertolini, an Assistant Professor in the Department of Mechanical Engineering at Politecnico di Milano, working in the research group led by Prof. Giorgio Colombo. During our discussion, Dr. Bertolini shared insights about his collaboration with Dr. Claudio Capelli to address the challenges of MR and the complex treatment they’re supporting with their training simulator model for TEER. He started working on the model as a Ph.D. student during a research period at the Institute of Cardiovascular Science at UCL in London, following a request from clinicians who could not find a proper solution to train for this procedure in the market. The solutions available are either too simplified, complex, or expensive. He adds, “Our goal was to create a realistic but easy-to-use, portable, and affordable solution as training and experience are crucial for achieving optimal outcomes and minimizing complications.”
Designing the 3D-printed simulator
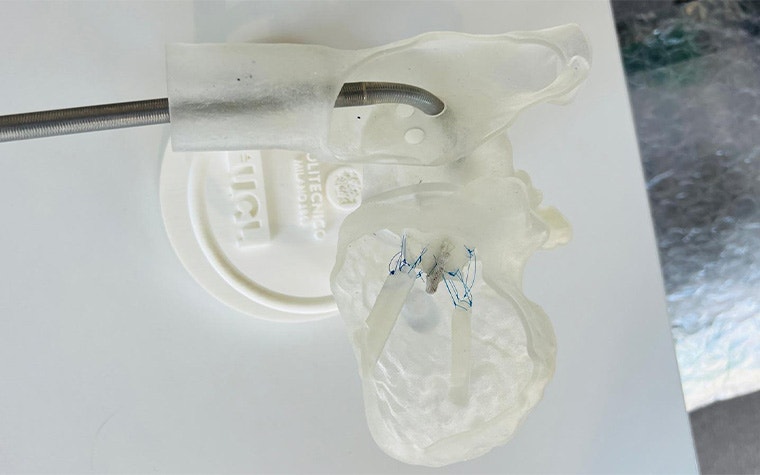
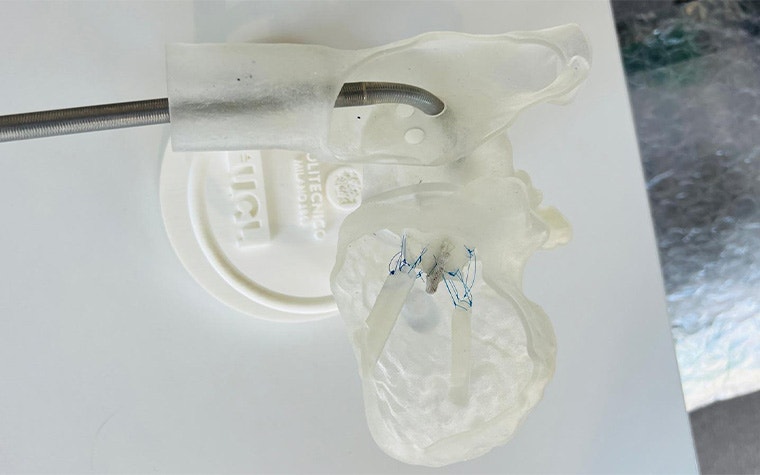
With this in mind, the team started with a representative CT scan dataset segmentation, as training on a realistic 3D-printed heart model adds the most value. Using Mimics, they segmented the atria and left ventricle from the blood pool. Then, using 3-matic, they edited the model and added features not fully visible on the CT scan, like papillary muscles, before designing the TEER training platform, including an interchangeable mitral valve model, holes for transseptal puncture, and baseplate. Lastly, they 3D-printed the model using a Stratasys PolyJet printer and proper soft-touch resins. The team has recently protected the simulator design with patents in the EU and UK.




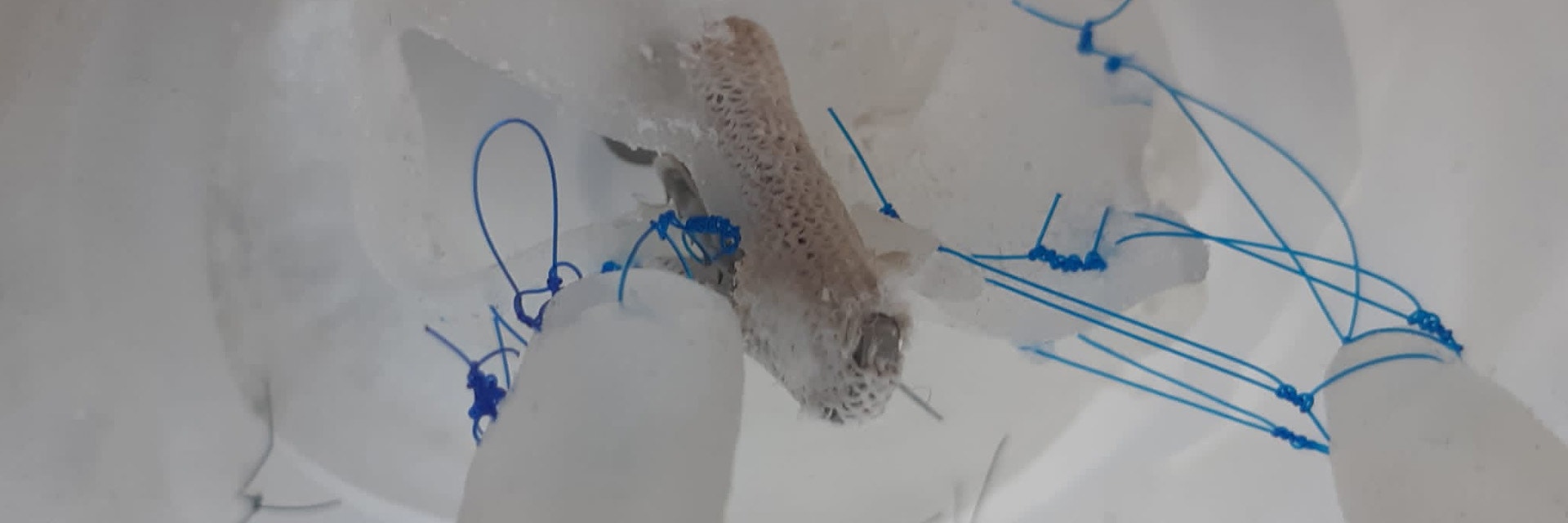
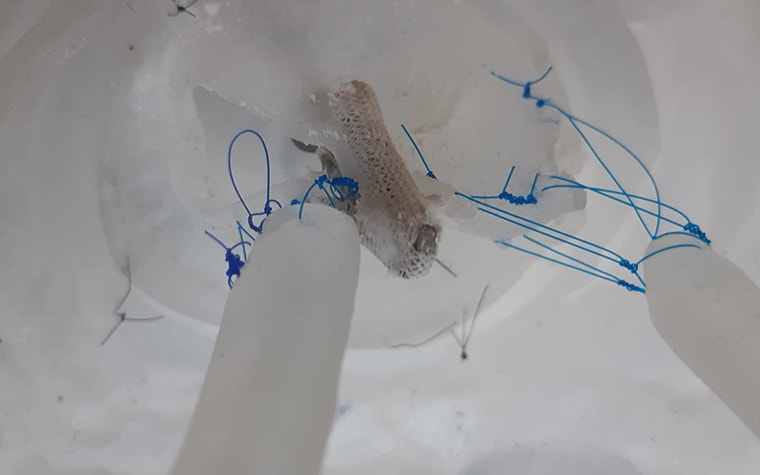
TEER simulator testing shown — I: Preparation, II: Guide insertion, III: Positioning of the clip, IV: Implantation
A significant increase in clinician confidence
To test their simulator, they approached 18 clinicians from four centers, with the help of Angel Babu, an assisting medical student, to use it and complete a questionnaire. Out of these clinicians, 8 already had experience completing TEER procedures. The study focused on determining the impact on trainees' confidence levels when they practice with a standard, idealized implantation model versus their designed, anatomically accurate solution. The procedure's most complex steps, such as steering the catheter, the transseptal puncture, and leaflet grasping, were evaluated for both models.
All clinicians' confidence in these essential parts of the TEER procedure significantly increased after training. Participants with no prior experience reported that the idealized model is beneficial for understanding maneuvers, while the experienced clinicians were more satisfied with the anatomical model. Dr. Bertolini adds, “The anatomical model helps clinicians apply the fundamental step or use the device to enhance problem-solving and safely navigating with the model’s border. So, rather than a model replacing the other, both models could be integrated into different stages of training.”
Applying the same work to other clinical practices
Dr. Bertolini and his team would like to complete a more systemic study with a randomized study protocol and a larger group of clinicians. They’d like to include more procedures in one simulator, such as merging other transcatheter heart valve procedures like TAVI so that clinicians can train different procedures with the same simulator. With their innovative work, it will be possible to create patient-specific heart models so that clinicians can train on the exact replica of the patient they will treat so that they can enter the CATH Lab with even more confidence.
L-103860-01
Materialise Mimics mentioned above is a research version only.
Materialise medical device software may not be available in all markets because product availability is subject to the regulatory and/or medical practices in individual markets. In countries where no regulatory registration is obtained of Mimics and/or 3-matic Medical, a research version is available. Please contact your Materialise representative if you have questions about the availability of Materialise medical device software in your area.
Share on:
You might also like
Never miss a story like this. Get curated content delivered straight to your inbox.