EXPERT INSIGHT
30 Years of Materialise: The Road Towards Mass Personalization

As Materialise is celebrating its 30th anniversary this year, we are looking back at the most meaningful innovations over the company’s history with a series of blog posts. In this post, we’re reflecting on some of our medical innovations as an example of our commitment to creating a better and healthier world.
3D planning for precise, personalized, and predictive insights
In the wide world of medical imaging, we have evolved from X-rays to the 3D-printed models of today. As of this historic era, clinicians can visualize their patients’ entire anatomy using 3D planning. And using 3D planning, clinicians can extract critical data that could be the difference for a patient needing a heart valve replacement. With the data, the patient could potentially qualify for a procedure that would improve their quality of life. This is just one of the ways that personalized healthcare is driving more predictable outcomes.
From the revolutionary X-Ray to 3D modeling
Let’s start at the beginning: X-rays were hailed as a medical miracle when discovered in 1895 — doctors could now see the inside of the body without surgery. It did not take long before the X-ray quickly became an important diagnostic tool. Radiologists and surgeons could review a patient’s images — and translate what they saw into a clear diagnosis and treatment path.
X-rays were the foundation of the field of medical imaging that eventually led to the development of computerized tomography (CT) scans in 1972, the first imaging modality capable of acquiring 3D images of a patient. Both modalities are still used today, but CT scans often form the building blocks of 3D modeling and allow us to create 3D applications.
As Pieter Slagmolen, Materialise Medical Innovation Manager, explains how this evolution in imaging has impacted therapy through planning, “If you look at planning in orthopaedics, the traditional paradigm is for a surgeon to use an X-ray, combine the information about the anatomy obtained from that X-ray with a patient’s clinical presentation and history, and rely on his training and a set of standard rules described in the literature to determine the optimal implant position. He then attempts to implement this plan as well as possible in the patient by using standard instruments to realize the plan he has in his head. While this is quick and easy, this approach often fails to handle the complexity of a patient’s anatomy. Leveraging 3D technology from medical images has created a broad range of possibilities to do much better.”
Shaping reality through medical engineering
With a background in biomechanics, Materialise’s founder Fried Vancraen saw an obvious link between sliced medical image data and 3D printing technology. The file that goes to a 3D printer is a stack of sliced 2D images. 3D medical images such as CT are mostly reconstructed as a stack of 2D images as well. Fried saw that link and then did the reverse — instead of slicing a file to get it ready for 3D printing, he took slices of a medical image to make a 3D model. This principle was the foundation of the Mimics software, which was launched in 1992. Today it continues to perform the digital ‘engineering on anatomy’ work, which forms the foundation of 3D printing workflows based on medical images.
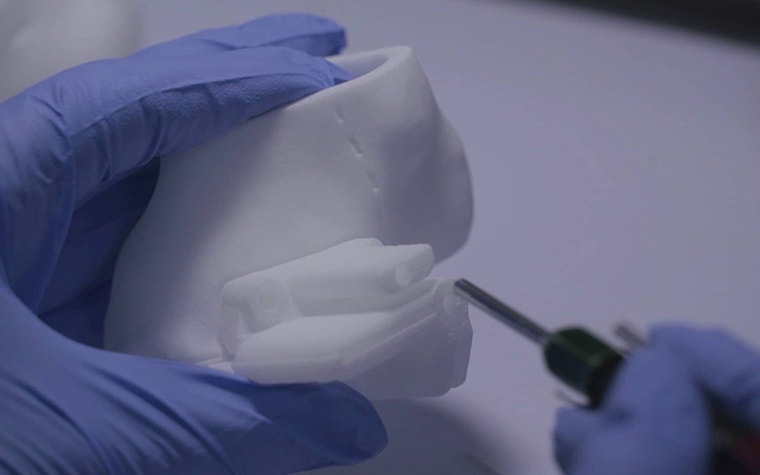
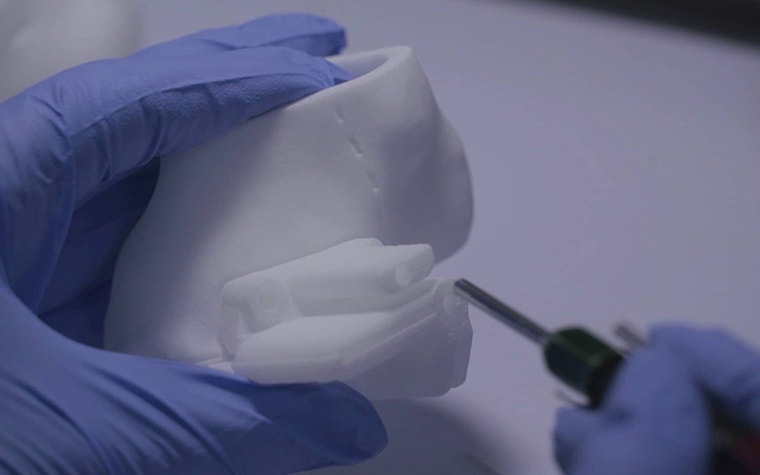
The 3D models that were created using slice image data from CT scans were the next step in this process. With the models, clinicians could then hold the exact replica of their patient’s anatomy to further their pre-procedural planning. In the following years, the models were able to be printed in different colors to further differentiate parts of the anatomy. These models helped clinicians to see the unseen more concretely and brought the medical imaging to life so they could better predict the issues they would encounter in the interventions. Eventually, with the advent of more powerful computers, doctors were able to access 3D visualization. This enabled the shift to virtual planning.
In 1996, Materialise focused on dental healthcare, creating the Materialise SimPlant software which allowed the surgeon to virtually plan their surgery before even looking at the patient. 3D-printed customized drill guides serve as the bridge between the virtual plan and the patient. The guides are able to accurately deliver the plan to the patient.
“Now you’re seeing much more planning happening based on 3D imaging where you can do 3D measurements or have a representation of the anatomy in hand, all based on 3D models. You're bringing in technology such as modeling or simulation just to extract more information out of the images that you have available and provide higher-quality planning and more predictability.”
— Pieter Slagmolen, Materialise Medical Innovation Manager
Shaping reality through FDA- and CE-certified tools
Hospitals across the world are steadily adopting medical 3D printing at the point of care to provide more personalized care on-site. This means that they are using their own machines to 3D print models to be used in pre-procedural planning. As regulators around the world came out with requirements for 3D software, Materialise took the initiative to get certified and became the first company with FDA and CE certifications. Pieter adds, “We want to ensure that we're helping our hospitals 3D print on-site in the best, most safe, and most qualitative way. So, for me, introducing the first software certified to create 3D-printed models for clinical use printed in a hospital setting is a highlight from recent years.”
The medical certifications demonstrate that Materialise has verified that the translation of the 3D model data to the printers can be accurate and that critical measurements will remain consistent, ensuring physicians can trust in the printed models.
Shaping reality for orthopaedic patients
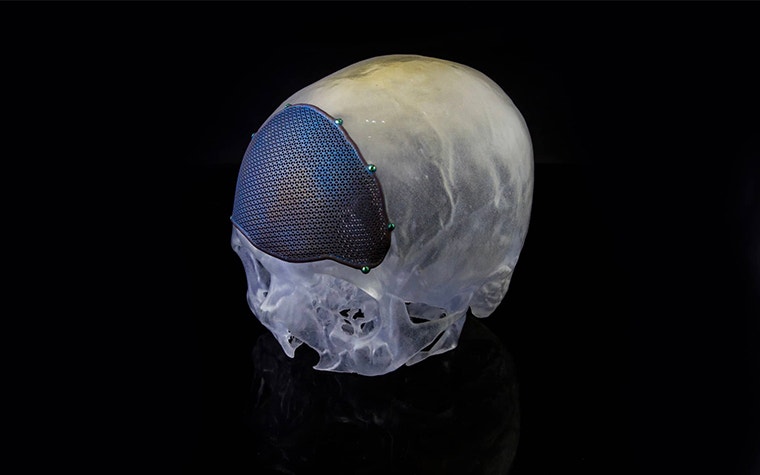
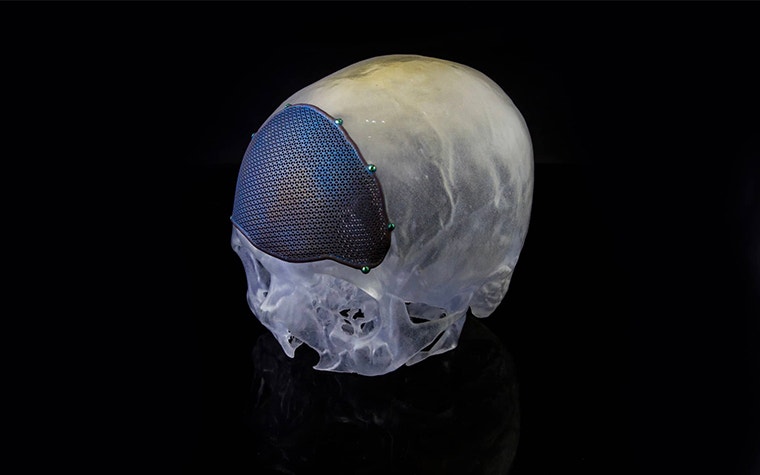
Between 2007 and 2008, the first hip and shoulder personalized implants were created for patients who had already had multiple revision surgeries. Since then, 3D planning has become an established way of supporting surgeons preparing for orthopaedic surgeries.
In a particular case, an 81-year-old man had already undergone hip revision surgeries and was no longer independently mobile. Collaborating with Materialise's clinical engineers, his orthopaedic surgeon was able to carefully plan his surgery upfront and design a 3D-printed aMace hip implant to achieve the desired mechanical reconstruction and fixation that was tailored to fit the defect. Using 3D planning, his surgeon was also able to pinpoint the exact drill positions so that the patient’s soft tissue would heal in the most optimal way.
Before surgery, the plastic bone model and implant trial served as a reference for the surgeon to prepare the site and position the implant correctly. After the surgery, the patient’s daughter reports that her father has gained his independence and that he says the successful surgery was better than winning the lottery!
Shaping reality for cardiovascular patients
3D planning has now entered the structural heart world, where it is continuing to make a significant impact on selecting the right patients, and preparing the optimal treatment plan for them. In particular, transcatheter mitral valve repair (TMVR) is a high-risk procedure in which a miscalculation of critical measurements could prove fatal for the patient. Usually, patients have multiple health issues to begin with, making them too high-risk to survive traditional surgery.
Antoon Dierckx, Materialise Medical Innovation Manager, clarifies, “Studies show that up to 50% of symptomatic patients who suffer from severe mitral defects are not referred to surgery because the expected surgical risk is just simply too high. But, with advanced 3D planning from Mimics Enlight, you can screen patients more effectively and include more viable cases, you can obtain insights on which implants would be optimal to use for that specific patient, and estimate to which extent the implant will impact blood flow through the heart. The outcome becomes more predictable and you can help a larger number of patients, who don’t have a lot of options otherwise.”
Now, with 3D planning in their toolbox, clinicians can treat more patients with powerful insights that support their critical decision-making.
“There could be great synergy between 3D planning, artificial intelligence, and augmented reality. With this, we will be able to further streamline a clinician’s workflow, and even further improve the predictability of patient outcomes.”
— Antoon Dierckx, Materialise Medical Innovation Manager
Shaping the future
Going forth, we see the trend continuing in more point-of-care medical 3D printing facilities in hospitals and clinics around the world. With certified software, they are better equipped to effectively prepare for cases on-site. We anticipate the power of 3D planning to spread to other fields after leaving its mark from dental to hip implants. After entering the complex structural heart world with TMVR, we see it continuing to other complex fields such as supporting lung cancer surgery.
Additionally, we see more interactions between technologies. Antoon explains, “There could be great synergy between 3D planning, artificial intelligence (AI), and augmented reality. With this, we will be able to further streamline a clinician’s workflow, and even further improve the predictability of patient outcomes.”
Today, surgeons can already view 3D plans and handle the visualizations within the operating room as 3D planning is already being integrated into augmented reality (AR). We envision that in the near future, the visualizations will be able to “recognize” the patient’s body and be able to direct the surgeon, for example, to exact drill locations. Taking one step further, 3D planning could also guide surgeons during robot-assisted surgeries. AI data sets will continue to grow, and surgeons will be able to personalize their preoperative plans to reflect the best outcomes for specific types of patients.
From the medical miracle of X-rays to today’s possibilities, medical imaging continues to inform surgeons and clinicians to make the best choices for their patients. As they can further personalize treatments for individual patients using 3D planning, treatment outcomes improve and become more predictable. After 30 years of innovation, our commitment to a better and healthier world is upheld by our dedication to further enhancing predictability.
L-101775-01
Share on:
You might also like
Never miss a story like this. Get curated content delivered straight to your inbox.
